Looking for women’s empowerment and personal healing work? Start here.
Better Healthcare for
Survivors
of Sexual Trauma
Invisible Wounds
Sexual trauma is shockingly common—and dangerously overlooked in clinical settings.


"Laura Zam's presentation about treatment gaps in women’s healthcare...was an incredible addition to our medical school curricula. Laura's knowledge...her personal story, and her fun interactive style helped our students learn concrete ways to better understand and serve their patients."
Claire Sandler,GW School of Medicine and Health Services,
The George Washington University
Invisible Wounds: What Sexual Trauma Survivors Need from Healthcare—But Rarely Get
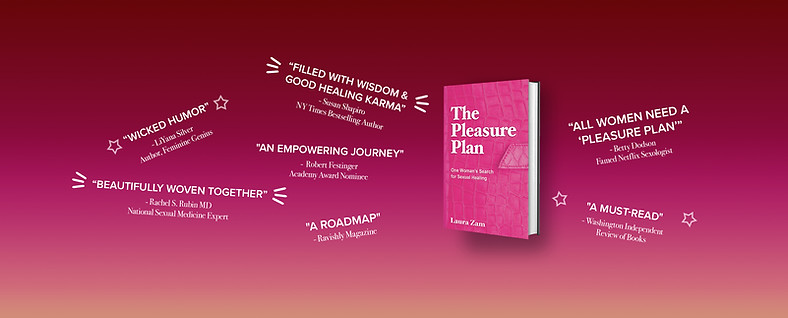
Drawn from Laura Zam's groundbreaking book The Pleasure Plan, Zam tells her story and offers concrete ways for medical professionals and mental health providers to fill in needed gaps in healthcare.
For 30 years, Laura Zam lived with pelvic pain and sexual dysfunction. She assumed the problem was her—a brokenness caused by childhood sexual abuse. Even when she disclosed this history on intake forms, providers rarely followed up. Not one asked how her trauma might affect a physical exam. What Zam didn’t know was that she had a very curable medical condition. Because no one connected her trauma history to her physical symptoms, she was repeatedly misdiagnosed—or dismissed altogether.
In this powerful keynote, Zam not only exposes the blind spots in survivor healthcare, she also gives providers indispensable tools to (1) recognize trauma’s hidden effects; and (2) respond in ways that are clinically sound, emotionally intelligent, and healing-centered.
This keynote is essential for anyone working in healthcare or mental health who wants to break the silence and offer care that facilitates full healing.
Learning Objectives:
By the end of this keynote, participants will be able to:
-
Understand how sexual trauma can present as physical pain, dysfunction, or shame—especially in female patients;
-
Recognize why survivors may not speak up—even when abuse is disclosed on intake forms;
-
Identify common provider blind spots that delay diagnosis, limit trust, or retraumatize patients;
-
Explore trauma-informed methods for intake, examination, and dialogue that enhance patient safety and clinician confidence;
-
Learn how to better support trauma survivors while protecting provider well-being.


